Break down the word “aerodigestive” and you can understand why the condition is so complex and intertwined. Children with aerodigestive conditions often have overlapping disorders involving the upper airway, larynx, trachea, esophagus and lungs, all of which originally developed embryonically from a common source.
One patient may have symptoms affecting multiple systems. At most pediatric hospitals, each condition is treated separately; subspecialists typically focus on the organ of their expertise and not the child holistically.
At Children’s of Alabama’s Aerodigestive Clinic, families don’t need to make multiple appointments and repeated trips to the hospital to see a slew of medical professionals. Instead, they can see a multidisciplinary team of pediatric subspecialists during a single clinic visit and receive coordinated care. Children’s Aerodigestive Program is the only one in Alabama and one of just a few around the country.
“We felt there was a big gap in care, and that led to frustrations that maybe we weren’t meeting their needs,” explained clinic coordinator Ashley Chapman of why Children’s started the program. Chapman focuses on improving communication and facilitating access.
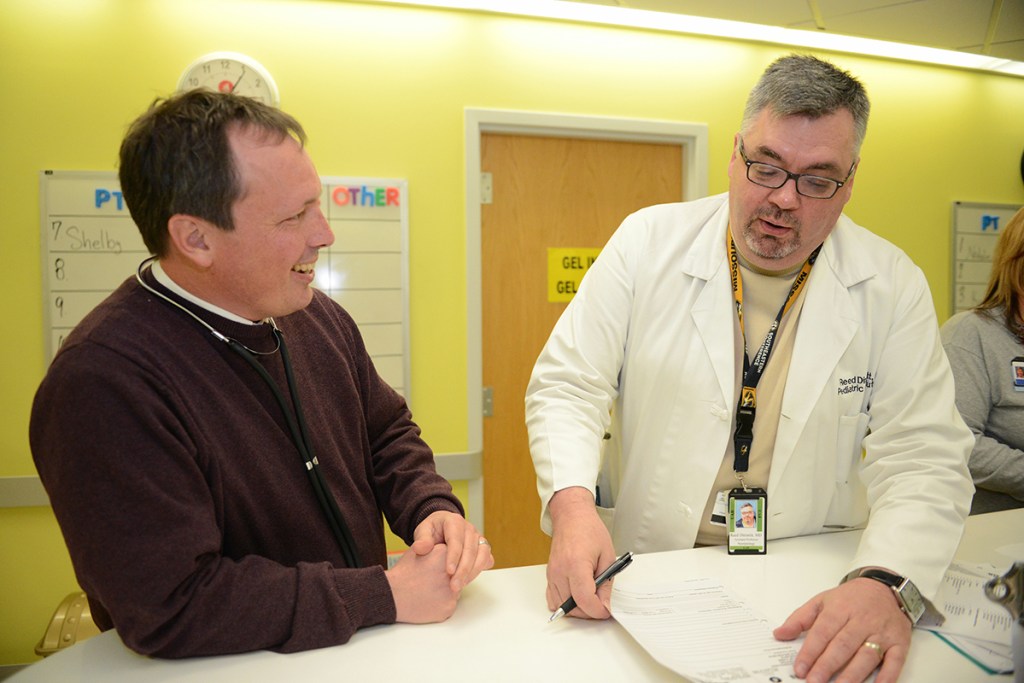
The result of better care has improved both patient and provider satisfaction. “Families appreciate that they don’t feel ‘bounced’ around the medical system,” said pediatric gastroenterologist Reed Dimmitt, M.D.
“Our team is a fun, collaborative group,” added pediatric pulmonologist Tom Harris, M.D. “Previously, we each treated the patients in a general clinic but were limited by our individual skill set. This approach allows us to lean on one another’s expertise, asking, ‘How can we improve care by working together?’”
Consider the triple endoscopy (direct laryngoscopy bronchoscopy, flexible bronchoscopy and esophagogastroduodenoscopy) with the ENT surgeon, pulmonologist and gastroenterologist all in the procedure room. Before, patients would need three separate procedures, requiring three times under general anesthesia with separate interpretations. Now, the three physicians meet together with the family post-procedure to discuss findings and deliver the management plan.
“It’s an additive model, but there’s also a synergy that occurs with everyone meeting together, which contributes to better outcomes,” said Dimmitt. “Collaborating with the multidisciplinary team,” he said, “pushes me to think outside the GI box.” The aerodigestive coordinator, speech pathologist and dietician are central to management plans, providing additional non-M.D. layers of coordination, expertise and pragmatic considerations.
The clinic offers in-person as well as telemedicine visits, and is growing fast, with referrals doubling in the past two years. “That’s also led to more complex patients,” added Dimmitt. “To meet these many needs, we spend a lot of time with the parents.”
The team receives referrals from a variety of sources, including inpatient subspecialists, community pediatricians and speech pathologists, among others. “My favorite referrals,” Harris said, “are families telling friends. That’s when we know we have succeeded.”
“What we hear from parents is that they are so thankful for the collaborative care, the time everyone spends and that their concerns are heard,” said Chapman.